In the realm of pediatric healthcare, identifying and mitigating risks, such as blood clots, is crucial for ensuring positive patient outcomes. Researchers at Vanderbilt University Medical Center (VUMC) developed a sophisticated artificial intelligence (AI) tool designed to predict blood clot risks in pediatric patients. Despite the tool’s high accuracy, clinicians displayed hesitancy in following its recommendations, leading to a deeper exploration of the challenges faced in AI implementation within healthcare settings. This article dives into the development of the AI tool, the clinical trial conducted to assess its effectiveness, and the critical insights gained from clinician responses, shedding light on the complexities of integrating AI into pediatric care.
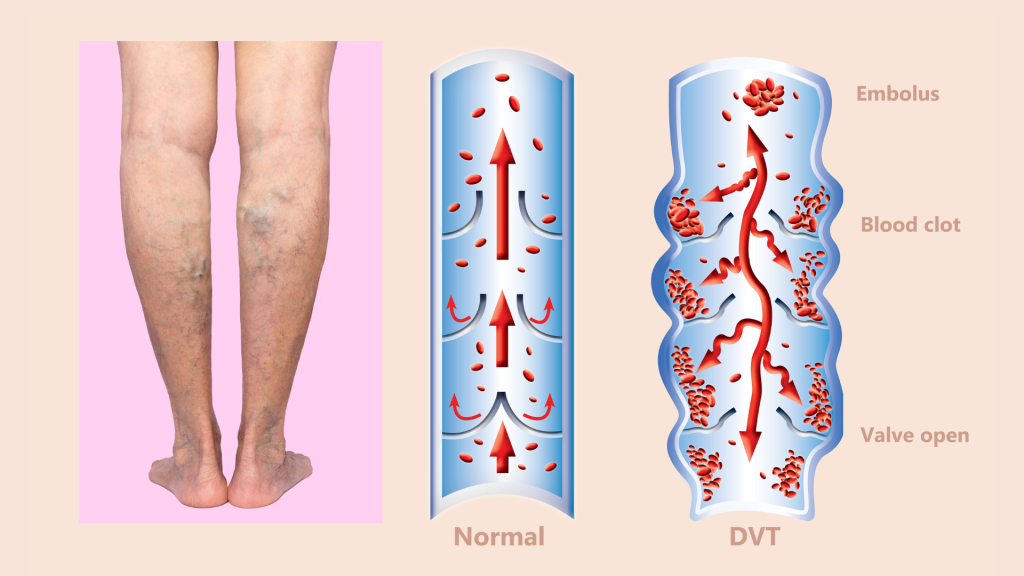
1. Addressing Pediatric Blood Clots:
Blood clots in pediatric patients, while rare, pose significant risks, including extended hospital stays and adverse outcomes. Recognizing the importance of early detection, researchers at VUMC utilized electronic medical records (EMRs) from the Monroe Carell Jr. Children’s Hospital to develop an AI algorithm. This tool aimed to identify high-risk patients by assessing 11 key factors associated with blood clot risks, paving the way for targeted interventions.
2. The Development and Trial of the AI Tool:
The research team meticulously analyzed patient data, leading to the creation of a predictive model. This model automatically assessed EMRs and calculated daily risk scores for each pediatric hospital admission. The AI tool’s efficacy was rigorously tested in the Children’s Likelihood of Thrombosis (CLOT) clinical trial, involving 17,000 patients. The study group received risk scores and AI-recommended anti-thrombolytic therapy, while the control group was managed by clinicians, allowing for a comparative analysis.
3. Clinician Reluctance and its Implications:
Despite the AI tool’s accuracy, clinicians hesitated to follow its recommendations. Concerns regarding potential bleeding complications influenced their decisions. This reluctance highlighted a critical barrier in AI implementation: the gap between AI-generated recommendations and clinician trust. The study emphasized that this reluctance did not stem from a failure of the AI model but rather from clinician apprehension.
4. Insights for the Future:
The study’s findings underscore the need for a comprehensive understanding of clinician perspectives when integrating AI tools into healthcare. To address this challenge, the research team is planning further clinical trials. These trials will focus on elucidating the barriers hindering clinician acceptance of AI recommendations. By examining these barriers, healthcare practitioners can develop strategies to enhance AI acceptance, ensuring that these advanced tools become integral components of patient care.
The VUMC study sheds light on the complexities of AI implementation in pediatric healthcare. While AI tools hold immense potential, the study emphasizes the importance of bridging the gap between technological advancements and clinician trust. By addressing clinician reluctance through thoughtful analysis and targeted interventions, healthcare providers can harness the power of AI to enhance patient outcomes, making strides toward a future where cutting-edge technology harmoniously coexists with compassionate and effective patient care.