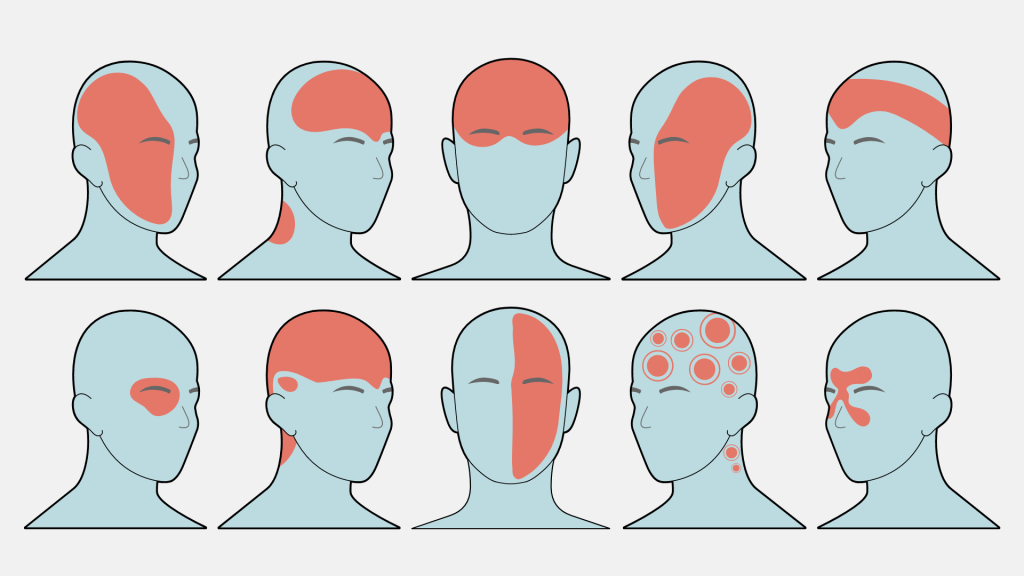
Migraines transcend mere headaches, presenting as a debilitating nervous system disorder. These episodes of agony, marked by intense throbbing pain, often on one side of the head, come hand in hand with nausea, vomiting, and heightened sensitivity to light and sound. Lasting hours or even days, sufferers seek refuge in dim, quiet spaces. Globally, around 800 million people endure these migraine attacks, with 39 million, or 12% of the U.S. population, regularly afflicted.
A striking gender divide exists: over three times as many women suffer from migraines compared to men. For women aged 18 to 49, migraines top the list of global disability causes. Research reveals that women’s migraines are not only more frequent but also more disabling and prolonged than those in men. Women tend to seek medical care and prescription drugs more often, and they often grapple with additional mental health challenges like anxiety and depression.
As a certified neurologist specializing in headache medicine, I’m captivated by the intricate gender dynamics of migraines. Unveiling these distinctions holds the key to understanding the complex interplay of hormones, genetics, epigenetics, and environmental factors that shape migraine experiences.
Hormonal Choreography:
Hormones like estrogen and progesterone wield considerable influence over the divergent migraine experiences of men and women. These hormones impact brain chemicals, possibly contributing to structural and functional brain differences linked to migraines. Estrogen and progesterone also regulate blood vessel size, potentially heightening susceptibility to migraine attacks.
While childhood sees equal migraine occurrence in both genders, puberty ushers in a change. Fluctuating sex hormone levels, particularly estrogen, increase migraine prevalence in girls. The hormonal rhythms of reproductive years amplify migraines further, with about 50% to 60% of women experiencing menstrual migraines. These menstrual migraines, triggered by estrogen level drops, are more severe and prolonged.
Aura and Its Enigma:
Migraine with aura adds intrigue with its visual and sensory symptoms preceding head pain. Visual disturbances, like dark spots and zigzag lines, herald an impending migraine. While aura mirrors certain stroke symptoms, its gradual onset distinguishes it from the abruptness of a stroke.
Life’s Milestones and Migraines:
Pregnancy brings a unique complexity as migraines intertwine with morning sickness. Pregnancy’s later stages may offer respite, though postpartum heralds a migraine resurgence. The transition to menopause unleashes a fresh chapter, as hormone fluctuations propel migraines during perimenopause. However, menopause often brings relief.
In men, migraines peak in the early 20s, taper off, then peak again around age 50 before slowing down. Genetics, environment, and lifestyle contribute to this distinctive pattern.
Pioneering Progress:
Bridging the gender gap in migraine research empowers women and advances global migraine understanding. Each discovery takes us closer to unraveling the complexity of migraines, offering hope to millions.