
What You Should Know About Psoriasis Symptoms
By Khrystyana Kirton
Edited by Stephanie Dawson
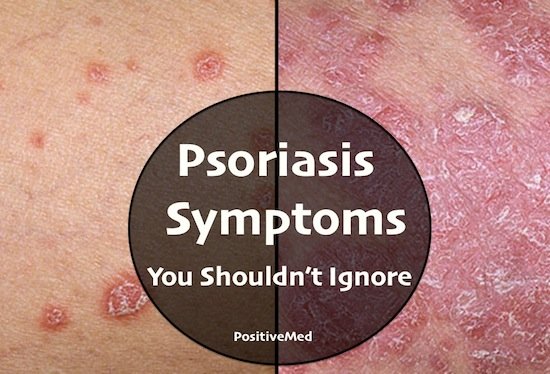
Psoriasis is a common skin disease that affects the life cycle of skin cells. Psoriasis causes cells to build up rapidly on the surface of the skin, forming thick silvery scales and itchy, dry, red patches that are sometimes painful. This is a persistent, long-lasting (chronic) disease. There may be periods when the psoriasis symptoms improve or go into remission alternating with times it worsens. For some people, psoriasis is just a nuisance. For others, it’s disabling, especially when associated with arthritis. There’s no cure, but psoriasis treatments may offer significant relief. Lifestyle measures, such as using nonprescription cortisone cream and exposing skin to small amounts of natural sunlight, can improve psoriasis symptoms.

Psoriasis signs and symptoms can vary from person to person but may include one or more of the following:
- Red patches of skin covered with silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
Psoriasis patches can range from a few spots of dandruff-like scaling to major eruptions that cover large areas. Mild cases of psoriasis may be a nuisance; more severe cases can be painful, disfiguring, and disabling.

Most types of psoriasis go through cycles, flaring for a few weeks or months, then subsiding for a time or even going into complete remission. In most cases, however, the disease eventually returns.
Several types of psoriasis exist. These include:
-
- Plaque psoriasis. The most common form, this type causes dry, raised, red skin lesions (plaques) covered with silvery scales. The plaques itch or may be painful and can occur anywhere on the body, including genitals and the soft tissue inside of the mouth. There may be a few plaques or many and, in severe cases, the skin around the joints may crack and bleed.

-
- Nail psoriasis. Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth, and discoloration. Psoriatic nails may become loose and separate from the nail bed (onycholysis). Severe cases may cause the nail to crumble.
- Scalp psoriasis. Psoriasis on the scalp appears as red, itchy areas with silvery-white scales. This is usually noticed when flakes of dead skin appear in the hair or on the shoulders, especially after scratching the scalp.
- Guttate psoriasis. This primarily affects people younger than 30 and is usually triggered by a bacterial infection such as strep throat. It’s marked by small, water-drop-shaped sores on one’s abdomen, arms, legs, and scalp. The sores are covered by a fine scale and aren’t as thick as typical plaques are. One may have a single outbreak that goes away on its own, or there may be repeated episodes, especially if there are ongoing respiratory infections.
- Inverse psoriasis. Mainly affecting the skin in the armpits, in the groin, under the breasts and around the genitals, inverse psoriasis causes smooth patches of red, inflamed skin. It’s more common in overweight people and is worsened by friction and sweating.
- Pustular psoriasis. This uncommon form of psoriasis can occur in widespread patches (generalized pustular psoriasis) or in smaller areas on hands, feet or fingertips. It generally develops quickly, with pus-filled blisters appearing just hours after the skin becomes red and tender. The blisters dry within a day or two but may reappear every few days or weeks. Generalized pustular psoriasis can also cause fever, chills, severe itching, and fatigue.
- Erythrodermic psoriasis. The least common type of psoriasis, erythrodermic psoriasis can cover the entire body with a red, peeling rash that can itch or burn intensely. It may be triggered by severe sunburn, by corticosteroids and other medications, or by another type of psoriasis that’s poorly controlled.

- Psoriatic arthritis. In addition to inflamed, scaly skin, psoriatic arthritis causes pitted discolored nails and the swollen, painful joints that are typical of arthritis. It can also lead to inflammatory eye conditions, such as conjunctivitis. Symptoms range from mild to severe, and psoriatic arthritis can affect any joint. Although the disease usually isn’t as crippling as other forms of arthritis, it can cause stiffness and progressive joint damage that in the most serious cases may lead to permanent deformity.
A variety of factors — ranging from emotional stress and trauma to streptococcal infection — can cause an episode of psoriasis. Recent research indicates that some abnormality in the immune system is the key cause of psoriasis. As many as 80% of people having flare-ups report a recent emotional trauma, such as a new job or the death of a loved one. Most doctors believe such external stressors serve as triggers for an inherited defect in immune function. Injured skin and certain drugs can aggravate psoriasis, including certain types of blood pressure medications (like beta-blockers), the anti-malarial medication hydroxychloroquine, and ibuprofen (Advil, Motrin, etc.)
Psoriasis tends to run in families, but it may skip generations, for example, a grandfather and his grandson may be affected, but the child’s mother never develops the disease. Although psoriasis may be stressful and embarrassing, most outbreaks are relatively harmless. With appropriate treatment, symptoms generally subside within a few months.





